Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Update on COVID-`9/Long Covid 19 how to Reorganize its Research Using AI Framework
*Corresponding author:Jorge Garza-Ulloa, Research Consultant Services, United States, University of Texas El Paso, USA
Received:July 07, 2022; Published: August 11, 2022
DOI: 10.34297/AJBSR.2022.16.002294
Abstract
From the start of the COVID-19 pandemic until today more than 2 million SARS-CoV-2 genome sequences has been generated and shared that inform about the outbreak control, disease surveillance, and public health policy [1]. The “probable future of COVID-19 that many scientists now fears are that is a virus that shows no signs of disappearing based on variants detected, where they adept by moving of the way to avoid the human body’s defenses”. The most important behavior observed is that the “coronavirus evolved by adaptation to reinfect people, taking us to being all our effort to be prepared for long-term patterns of virus survive among us by now seems that the probability of having different waves of two or more infections a year it is possible”. An “additional important is the accumulative problem of millions of COVID-19 people that survived the infection shows long COVID-19 symptoms”.
One factor that contributes to COVID-19 is “cytokine storm” emanating from macrophages because of unregulated inflammation in and around lung epithelial and endovascular cells. Besides, neurological aftereffects such as “anxiety” and “brain fog” are becoming a major issue for both the pandemic and post-pandemic period. This research paper has the goal to concentrate important information to summarize discovers, treatments, classification, methods, and proposed techniques of many medical specialized doctors, health personnel and researchers around the word to help on the now necessary fast adaptation on the fighting of this virus. With the main objective to propose a reorganization for the “COVID-19/long COVID-19 research analyzing with multidiscipline care using Artificial intelligence (AI) under a revolutionary computing clouding mainframe” that can organize and follow-up all datasets under a new concept named: “Personalized health for medical precision (PHMP)”, that will simplify detection, follow-up, progression analysis, and even prediction under two processing types: “traditional” and “PHMP”. In the “traditional processing” all data is compared with other patients to define a health range calculated applying general statistics and on “PHMP” is analyzed only with all the information of one patient and his datasets using “intelligent and configurable database” of the COVID- 19 patients including genetic data.
COVID-19 (SARS-CoV-2) Biggest Issues
The “Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)”, it is the virus which causes COVID-19, and identify as the cause of an outbreak of respiratory illness first detected in Wuhan, China in 2019. COVID-19 at the beginning was classified only as a “respiratory condition caused by the coronavirus”, COVID-19 affects different people in different ways:
a.Some people are infected but does not show any symptoms identified as “asymptomatic”. Most people will have mild symptoms and get better on their own.
b.Some will have severe problems, such as “trouble breathing”.
c.The odds of more serious symptoms are higher if you’re older or have another health condition As: diabetes, heart disease or a disease that weakens their immune system.
d.The most common things people who become ill with COVID-19 have include fever or chills, dry cough, and shortness of breath, feeling very tired, muscle or body aches, headache, loss of taste or smell, sore throat, congestion or runny nose, nausea or
vomiting, diarrhea, and other symptoms. They can start anywhere
from 2 to 14 days after having contact with the virus.
e. But a big number of problems are accumulating over the
time with the new variants after infection with the Coronavirus
SARS-CoV-2 better identified as “post-COVID-19 syndrome or long
haulers COVID-19 or long COVID-19”, where all infected persons
may suffer severe physical and mental affectation presenting a big
variety of neurological symptoms and others [2]. According to the
“Centers for Disease Control (CDC) (CDC)”: “long COVID” may also
be referred to as “long-haul COVID”, “post-acute COVID-19”, “longterm
effects of COVID or chronic COVID”. The reality is that is an
urgency to reorganize the research of COVID-19/post-Covid-19 to
find answers. Until today there are only hypothesis to explain the
“post-Covid-19” [3]:
i. “A persistent virus or viral remnants in tissues”, such as
viral RNA or protein could be triggering chronic inflammation.
ii. “Autoimmunity”, an acute respiratory infection can induce
autoimmune conditions for damage in some patients. Once this
happens, it is difficult to reverse.
iii. “Dysregulated gut microbiome, dysbiosis and latent
reactivation of viruses” such as Epstein-Barr infection.
COVID-19 evolved continuously and the necessity of understand
SARS-CoV-2 most important COVID issues until now are “genome”
and “actual keys”. Where:
a. “genome” defined as spans of DNA sequence
b. “Continuously evaluation of coronavirus actual keys” to
inform of local outbreak and understand national trends, “related
variants”, “COVID variants behaviors”
Genome for SARS-CoV-2
The SARS-CoV-2 genome consists of 15 “open reading frames (ORFs)” that are defined as spans of DNA sequence between the start and stop codons (a studied region of a single-celled organism that lacks a nucleus of a DNA sequence) coded into 29 proteins. SARS-CoV-2 has four main structural proteins that are important for coronavirus infectivity as shown in Figure 1: “Membrane-M protein”, “Nucleocapsid-N protein”, “Spike-S protein” and “Envelope-E protein” [4]. Where their basic functions are: (Figure 1)
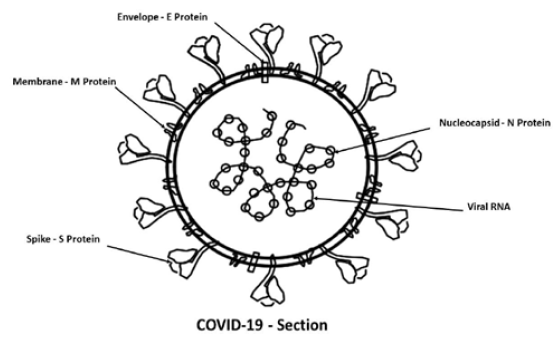
Figure 1: COVID-19 section view showing its 4 main proteins for infection: “M protein”, “N protein”, “S protein” and “E protein”.
a. “Nucleocapsid-N protein” or “protein chaperones”
that protects the viral RNA genome, it is one of the most crucial
structural components of SARS-CoV-2*. The “N protein of SARSCoV-
2” is encoded by the ninth ORFs of the virus and is composed
of 419 amino acids.
b. “Spike-S protein” are spikes consisting of three copies of
the “S glycoprotein” that promote receptor-binding**. It is used as
entry with “S1 subunit” for binding to a host cell receptor, and “S2
subunit” for fusion of viral and cellular membranes.
c. “Membrane-M protein” is an integral membrane that
adapts a region for virus assembly and capture other structural
proteins at the budding site***.
d. “Envelope-E protein” is a small integral membrane
protein, it is present in sub- stoichiometric amounts and acts as an
enhancer of budding that adapts a region of membrane for virus
assembly and captures other structural proteins at the budding
site. It is involved in many aspects of the viral life cycle**** [5].
*The “N protein” of SARS-CoV-2 is highly immunogenic and is expressed abundantly during infection by replication and transcription. This protein shares 90% homology with the severe acute respiratory syndrome coronavirus “N protein”, implying functional significance [6].
**“Spike glycoprotein” is highly immunogenic, and antibodies against spike glycoprotein are found in patients recovered from SARS and COVID-19. The spike protein is responsible for viral entry into the host cell, a required early step in viral replication.
***“M protein” is related to viral infectivity through binding to the viral “S protein” and the “host surface receptor(s)”, thus promoting membrane fusion. It plays a central role in virus assembly, turning cellular membranes into workshops where virus and host factors come together to make new virus particles.
****The “E protein” promotes the packaging and reproduction of the virus, and deletion of this protein weakens or even abolishes the virulence.
A comprehensive understanding of all these proteins should prompt further studies on the design and characterization of effective targeted therapeutic measures.
Actual Keys of SARS-CoV-2
The actual keys to inform local outbreak and understand national trends, scientists compare differences between virus evolutions in the genetic code caused by genetic mutations or viral recombination to identify variants including recombinants. These are based on related of 4 keys observations by CDC: “Mutation”, “Recombinant”, “Linage”, and “Variant” [7].
a. “Mutation” is a single change in a virus code also known
as genetic code*.
b. “Recombinant” is the process in which the genomes of
two SARS-CoV-2 variants that have infected a person at the same
time combine during the viral replication process to form a new
variant that is different from both parents’ lineages.
c. “Linage” is a group of closely related viruses with a
common ancestor**.
d. “Variant” is a viral genome (genetic code) that may
contain one or more mutations. “Variants” are classified due to
shared attributes and characteristics that may require public health
action as: “Variant being monitored”, “Variant of Interest”, “Variant
of Concern”, and “Variant of high consequences”. Where their
descriptions are:
i. “Variant being monitored (VBM)” is a category for current
variants that are monitored and characterized by federal agencies.
ii. “Variant of Interest (VOI)***” is when specific genetic
markers are predicted to affect transmission, diagnostics,
therapeutics, or immune escape. Additionally, there are evidence
that is the cause of an increased proportion of cases or unique
outbreak clusters.
iii. “Variant of Concern (VOC)***” is a category used for
variants of the virus where mutations in their spike protein
receptor binding domain substantially increase binding affinity,
while also being linked to rapid spread in human populations
(epidemiological data) [8].
iv. “Variant of high consequences (VOHC)” is a category for
Variants with certain genetic substitutions in the spike -S protein,
that is key to how the virus sticks to and infects cells are being
monitored for such resistance and interference with vaccines
designed to provide immunity and does not is affected by current
treatments.
Examples for SARS-CoV-2 actual keys [9]:
a. On April 14, 2022, the U.S government SARS-CoV-2
Interagency Group (SIG) “downgraded Delta from a Variant of
Concern to a Variant Being Monitored”. This new classification was
based on the following:
i. Significant and sustained reduction in its national and
regional proportions over time.
ii. Evidence suggesting that Delta does not currently pose a
significant risk to public health in the United States.
b. On May 17- 2022, the “variants of concern****” are:
I. “Omicron B.1.1.529, BA.1, BA.1.1, BA.2, BA.3, BA.4* and
BA.5* lineages”. First identify in South Africa. The main Omicron
characteristic [10]:
i. Spreads more easily than other variants.
ii. Severe illness and death: Data suggest that Omicron is less
severe in general. However, a surge in cases may lead to significant
increases in hospitalization and death.
iii. Vaccine: Breakthrough infections in people who are
vaccinated are expected but being up to date on recommended
vaccines is effective at preventing severe illness, hospitalizations,
and death. The emergence of the Omicron variant further
emphasizes the importance of vaccination and boosters.
iv. Treatments: Some, but not all, monoclonal antibody
treatments remain effective against Omicron.
c. Scientists has notice that variants now seem to emerge
roughly every six months, but this is not a rule they have allow to
observe the behavior of SARS-CoV-2 [11], because these are the
“first signs that the virus is evolving differently” compared with the
first two years of the pandemic, when variants seemed to appear
out of nowhere.
COVID-19 typical stages shown the following stages:
a. “Infection” identified as an early COVID-19 viral
replication.
b. “Cytokine storm”, where “cytokines” are small, secreted
proteins released by cells that have a specific effect on the
interactions and communications between cells. They are very
important in the host defense system and play a critical role in
protection against bacterial and viral infections. “Cytokines” are
also involved in the pathogenesis and development of symptoms
in infections.
c. “Micro-thrombosis” [12], COVID-19 is associated with
a significant risk of thrombotic complications ranging from
microvascular thrombosis, venous thromboembolic disease, and
stroke. Importantly, thrombotic complications are markers of
severe COVID-19 and are associated with multiorgan failure and
increased mortality.
Please see COVID-19 updated information at cdc.gov:
SARS-CoV-2 Variant Classifications and Definitions (cdc.gov)
https://www.cdc.gov/coronavirus/2019-ncov/variants/variantclassifications.
html
Please see current coronavirus SARS-CoV-2 evolution based Phylogenetic relationships of “Next strain” SARS-CoV-2 common ancestor and all its lineal descendants on a phylogenetic tree known as “clades” for more info see www.covariants.org [13], and data from www.nextstrain.org [14].
*Mutations happen frequently, but only sometimes change the characteristics of the virus.
**SARS-CoV-2 has many lineages; all cause COVID-19.
***The World Health Organization (WHO) external icon also classifies variant viruses as “variants of concern” and “variants of interest”; U.S. classifications may differ from those of WHO because the impact of variants may differ by location. To assist with public discussions of variants, WHO proposed using labels consisting of the Greek alphabet (for example, alpha, beta, gamma) as a practical way to discuss variants for non-scientific audiences.
****“European Centre for Disease Prevention and Control (ECDC)” designated the “BA.4 and BA.5 Omicron subvariants as variants of concern (VOC)” and said they could fuel increases in infections in the region in the weeks and months ahead
Post-COVID Syndrome / Long Haulers COVID-19 / Long COVID-19
Today is know that during and after infection with the Coronavirus SARS-CoV-2 better identified as “post-COVID-19 syndrome or long haulers COVID-19 or long COVID-19”, where all infected persons may suffer severe physical and mental affectation presenting a big variety of neurological symptoms and others [2]. They are mainly caused by the infection with “severe damages by inflammation at the different organs of human body into the complex network of all symbiotic systems”.
Many of the symptoms has been documented for many patients with mild to moderate COVID-19, and they can last weeks to months and may be years with their virus symptoms. “Post-COVID patients” are identified by the fact that they had COVID-19 and they have tested negative but continue with many symptoms. Where “some people have reported feeling better for days or even weeks then relapsing.
Meanwhile, others report they are just not feeling like themselves”.
On this paper is proposed to study the “symbiotic systems under a multidisciplinary care system* affected by COVID-19 and post-COVID syndrome”.
*Multidisciplinary care is a unified group approach in a healthcare setting where the responsibility of plans of treatment and delivery of care doesn’t lie on a single person but a group of qualified professionals with different medical specialization.
Symbiotic Systems Affected by COVID and Post-COVID Syndrome
The “Long COVID” patients frequently suffer from multiorgan impairment” as detected on many research paper [15], then the COVID-19 & post-COVID syndrome muse be studied based on the interactions between them. The human symbiotic systems have many types of organs that have interdependency and alteration affected by post-COVID. They symptoms can be classified based on their affected organs into each symbiotic system. These are: “respiratory system”, “cardiovascular or circulatory system”, “nervous system”, “immune system”, “digestive system”, “excretory system”, “reproductive system”, “muscular system”, “lymphatic system”, “endocrine system”, and “integumentary system” [16]
Respiratory System
How respiratory system is affected:The “respiratory system” mainly by infection in the lungs, that carry out the exchanges of gases as we breathe, altering the amount of red blood cells that collect the oxygen from the lungs and carry it to the different parts of the body where is needed and collect the carbon dioxide that transport back to the lungs to be expelled from the body.
Post-COVID disease on respiratory system:“Pulmonary function deficit”, “Pulmonary Fibrosis, “Dyspnea”, others
How respiratory system affect others symbiotic systems:The decreases of the oxygen needed in the human body known as “hypoxia”, condition that affect the brain cells and initiate the process of brain damage and finally neurons death. When the virus gets in your body, it meets the mucous membranes that line nose, mouth, and eyes. The virus enters a healthy cell and uses the cell to make new virus parts. It multiplies, and the new viruses infect nearby cells. The “COVID-19” was first cataloged as a disease caused by “SARS-CoV-2” that can trigger a respiratory tract infection. It can affect your upper respiratory tract (sinuses, nose, and throat) or lower respiratory tract (windpipe and lungs). As “COVID-19 pneumonia” progresses, more of the air sacs become filled with fluid leaking from the tiny blood vessels in the lungs. Eventually, shortness of breath sets in, and can lead to “acute respiratory distress syndrome (ARDS)”, a form of lung failure [17]. For “post COVID is frequently the inflammation at lower and upper tracts for shortness of breath” [18].
Attention needed on the respiratory system research:Considerable attention is needed for “viral COVID-19 lung infection detections and track progression since early infection”.
Cardiovascular or Circulatory System
How cardiovascular or circulatory system is affected:The “cardiovascular or circulatory system” is affected mainly by inflammation in the heart, veins, arteries capillaries, etc. The heart and blood vessel work together to circulate the blood throughout the body to provide oxygen and nutrients as amino acids, electrolytes, carbon dioxide, hormones etc. this helps to fight diseases, stabilize temperature, acidity, or alkalinity (pH), and maintain “homeostasis” as the process to maintains a relatively stable equilibrium between interdependent elements, especially as maintained by physiological processes [16].
Post-COVID diseases on the cardiovascular or circulatory system:
I. Circulatory:
• “Arterial and venous thrombosis”, “Endothelial cell
dysfunction (ECD)”, “Elevated D-Dimer and C reactive protein
levels”, and others.
II. Cardiac symptoms:
• “Chest pain”, “Palpitations”, ”Myocardial injuries”, “Stress
cardiomyopathy”, “Cardiac arrythmias”, others.
How cardiovascular or circulatory system affects others symbiotic systemsSARS-CoV-2 has been demonstrated to interact with “ACE2 (Angiotensin-converting enzyme 2)”, that is an enzyme attached to the membrane of cells located in the intestines, kidney, testis, gallbladder, and heart, and enter the host’s cells, particularly cardiac myocytes, and alveolar epithelial cells [16,19]. The binding of SARS-CoV-2 to “ACE2” causes acute myocardial and lung injury through the alternation in “ACE2” signaling pathways [20].
Attention needed on the cardiovascular or circulatory system research:Considerable attention is needed for viral infection related heart damage at the time of treatment. The cardiologist community must play an essential role in managing and treating patients affected by this disease. For “post COVID symptom is frequently the inflammation in the heart (causes acute myocardial), veins, arteries capillaries” [21].
Nervous System
How nervous system is affected:The “nervous system” is affected by COVID-19 virus in the brain, and extents the inflammation also to the spinal cord, nerve cells and all nerves that connect these organs with the rest of the human body. The brain and the spinal cord form the “central nervous system (CNS)”, where the information is evaluated, and decision are made and send them to the “sensory nerves” or by vice versa in the “sensory organs” information are send to them [22].
Post-COVID disease on the nervous system:The nervous system express affectation through: Headache, Fatigue, Hyposmia, Cognitive impairment, Sleep disorders, Pain, Guillen Barrie syndrome, Psychiatric symptoms, and many others.
How nervous system affects others symbiotic systems:The different nerves affected that carry signals to/from muscles, glands, and organs are responsible for regulate their normal functions and cannot achieve the equilibrium between interdependent elements in the human body and the disease [23].
Attention needed on the nervous system research:Describing the different neurological conditions that may occur in COVID-19 patients and how to diagnose them, as well as likely pathogenic mechanisms. This is key to direct appropriate clinical management and treatment [24].
Immune System
How immune system is affected:The “immune system” accomplishes its responsibility for the body´s defense against infectious organisms and other invaders. After people recover from infection with a virus, the “immune system” retains a memory of it. Normally the immune cells and proteins that circulate in the body can recognize and kill the pathogen if it is encountered again, protecting against disease, and reducing illness severity. This long-term immune protection involves several components. “Antibodies” as proteins that circulate in the blood that recognize foreign substances like viruses and neutralize them. Different types of “T cells” that help recognize and kill pathogens. “B cells” make new antibodies when the body needs them [25]. All these immunesystem components have been found in people who recover from SARS-CoV-2, the virus that causes COVID-19. But the details of this immune response and how long it lasts after infection have been unclear [26].
Post-COVID disease on the immune system:The immune system overreacts to the virus, triggering an aberrant innate immune response that is characterized by systemic inflammation, intravascular blood clotting and damage to the cardiovascular system [27].
How immune system affects others symbiotic systems:The initial decisions of the innate immune system are responsible for a proper or improper response of the adaptive immune system and, along with comorbidities, are directly associated with disease progression.
Attention needed on the immune system research:The initial decisions of the innate immune system are responsible for a proper or improper response of the adaptive immune system and, along with comorbidities, are directly associated with disease progression. Special attention is needed on how to improve the initial decision of the immune system.
Digestive System
How digestive system is affected:“Digestive system” as a group of organs working together to convert food into energy and basic nutrients to feed the entire body. The alimentary canal is made up of the oral cavity, pharynx, esophagus, stomach, small intestine, large intestines an anus. Accessory organs of the digestive system include: the teeth, tongue, salivary glands, liver, gallbladder, and pancreas. In some instances, digestive symptoms are reported as the initial presentation of COVID-19 [28]. These findings suggest that the virus can impair the digestive system and may explain the range of digestive symptoms seen in COVID-19. Digestive symptoms should be treated with caution in the early stage of COVID-19, and “dynamic monitoring of liver function and cytokines” is imperative during clinical practice to reduce the complications and mortality of COVID-19. The most common symptoms are “anorexia and diarrhea”. In about half of the cases, viral RNA could be detected in the stool, which is another line of transmission and diagnosis. Compared with patients without gastrointestinal sequelae at 90 days, patients with gastrointestinal sequelae more frequently presented with “dyspnea (difficult breathing)” and “myalgia (Muscle pain)” on admission. “In long post COVID-19 symptoms reports: diarrhea, nausea, vomiting, and diminished appetite even after 90 days” [29]
Post-COVID disease on the digestive system:The most frequently Post-COVID Symptoms are diarrhea, vomiting, belly pain, lack of appetite, loss of taste and smell, vomiting up blood or gastro-Intestinal bleeding, belching, acid reflux, indigestion, and others [30].
How digestive system affects others symbiotic systems:Once any virus infects your body, it can destroy healthy cells and make multiple copies of itself. COVID-19 mainly attacks the cells lining your airways. This makes it hard for you to breathe and can lead to pneumonia, besides destroy bowel tissues, and reduce intestinal movement. But researchers think the illness also may harm your digestive tract and liver tissue.
Attention needed on the digestive system research:Digestive symptoms were more likely to have a positive stool test for the coronavirus, which means they had SARS-CoV-2 RNA in their digestive system. It also took them longer to clear the virus from their bodies, compared to those without gastrointestinal symptoms. Some research shows that SARS-CoV-2 enters intestinal cells and respiratory cells using the “angiotensin-converting enzyme 2 (ACE-2) protein” as a receptor. The “ACE-2 receptor” is embedded in cellular membranes. It helps regulate blood pressure by controlling levels of the protein angiotensin, which encourages blood vessels to constrict and raise blood pressure.
When SARS-CoV-2 particles leave an infected cell, it triggers the release of “cytokine that are small proteins that play a role in inflammation”. This process may cause gastrointestinal (GI) symptoms with up to one-third of patients with COVID-19 presenting first with GI symptoms. Nausea and vomiting may be present in up to two-thirds of patients with COVID-19. When the virus enters intestinal cells after its characteristic spike proteins bind to ACE-2. Once inside the cell, the virus uses the cells’ own machinery to produce copies of viral proteins and RNA. Like many viruses, SARS-CoV-2 carries its genetic information on a strand of RNA, much like human DNA. More research is needed [31].
Excretory System
How excretory system is affected:“Excretory system” includes the renal system that consists of kidneys, ureters, bladder, and the urethra. The purpose of the renal system is to eliminate wastes from the body, regulate blood and blood pressure, control levels of electrolytes e.g., sodium, potassium and calcium, and metabolites, and regulate blood pH that indicates the acidity or alkalinity. Urine is formed in the kidneys through a filtration of blood. The kidneys have an extensive blood supply via the renal arteries which leave the kidneys via the renal vein.
Post-COVID disease on the excretory system:Kidney damage
three most-common kidney lesions are:
i. “Acute tubular necrosis” is a medical condition involving
the death of tubular epithelial cells that form the renal tubules of
the kidneys.
ii. “Collapsing glomerulopathy” a is associated with marked
proteinuria, rapid decrease in kidney function, and a poor prognosis.
iii. “Thrombosis” is formation or presence of a blood clot in
a blood vessel.
This post-COVID19 lesion are made for the virus itself infects the cells of the kidney as “Cytokine storms” that can destroy kidney tissue. Kidney cells have receptors that enable the new coronavirus to attach to them, invade, and make copies of itself, potentially damaging those tissues. Similar receptors are found on cells of the lungs and heart, where the new coronavirus has been shown to cause injury [32].
How excretory system affects others symbiotic systems:
The impact of COVID-19 on the kidneys is complex. Here are some
possibilities doctors and researchers are exploring [33] are:
i. “The virus itself infects the cells of the kidney”. Kidney
cells have receptors that enable the new coronavirus to attach to
them, invade, and make copies of itself, potentially damaging those
tissues. Similar receptors are found on cells of the lungs and heart,
where the new coronavirus has been shown to cause injury.
ii. “Abnormally low levels of oxygen in the blood”. Another
possibility is that kidney problems in patients with the coronavirus
are due to “abnormally low levels of oxygen in the blood”, a result of
the pneumonia commonly seen in severe cases of the disease.
iii. “The body’s reaction to the infection” may be responsible
as well. The immune response to the new coronavirus can be
extreme in some people, leading to what is called a “cytokine storm”.
iv. “COVID-19 can cause tiny clots to form in the bloodstream,
which can clog the smallest blood vessels in the kidney and impair
its function”. The kidneys are like filters that screen out toxins, extra
water, and waste products from the body.
Attention needed on the excretory system research:Up to 87% of patients hospitalized with coronavirus disease 2019 (COVID-19) experience chronic sequelae following infection. The long-term impact of COVID-19 infection on kidney function is largely unknown at this point in the COVID-19 pandemic [33]. The impact of COVID-19 on the kidneys is not yet clear. More research must be focus on the COVID-19 damage to the excretory system.
Reproductive System
How reproductive system is affected:“Reproductive system” is a system of sex organs within an organism which work together for the purpose of sexual reproduction. Many substances such as fluids, hormones and phenomes are also important accessories to the reproductive system. The combination of genetic material between two individual of different sex allows the possibility of greater genetic fitness of the young born of living organisms. SARSCoV- 2 has been demonstrated to interact with “ACE2”, where “ACE2 receptors” are much more abundant in the male reproductive system than the female reproductive system. Low expression of “ACE2” was demonstrated in the fallopian tube (ciliated and endothelial cells), ovary, vagina, cervix, and endometrium. On the other hand, “ACE2” expression in the testis is among the highest observed, with high expression in “Leydig and Sertoli cells and medium expression in glandular cells of the seminal vesicle”. As a result, it is expected that the testes will be more vulnerable than the ovaries to the detrimental effects of a SARS-CoV-2 infection. In females, a severe acute illness may alter the “hypothalamic-pituitary gonadal (HPG) “axis function, decreasing the endogenous production of “estrogens and progesterone” [33].
Post-COVID disease on the reproductive system:Scientific findings related to the impact of the COVID-19 pandemic on the reproductive process, considering gender, hormonal balance, gonad functions, pregnancy, and assisted reproductive technology (ART). The sociosexual dimension of COVID-19 disease and precautions that should be taken to avoid infection via sexual transmission or vertical transmission, which may alleviate the fear associated with continuing normal social relationships and economic activities [29].
How reproductive system affects others symbiotic systems:Long post COVID-19 report a high frequency of maternal mental health problems, such as clinically relevant “anxiety and depression”, but these are consequences of social- economic problems affected by the pandemic as fear of putting your own and your child’s health at risk to go to a clinic or medical facility comes into play, increased childcare demands and other factors. The pandemic has shifted perspectives on family planning, likely due to the diverse impacts of COVID-19, including loss of health insurance and income [34].
Attention needed on the reproductive system research:Special research must be done on “COVID-19 Mother to baby” [35]
a. “Placentitis” COVID-19 infect the placenta, which can
lead to problems with how well the placenta works to support the
pregnancy and the baby’s growth and development. Researchers
are learning more about other possible effects of “placentitis”
caused by a COVID-19 infection.
b. “Pregnancy increase change of becoming very sick of
COVID-19” people who are pregnant or recently pregnant have a
higher chance of becoming very sick from COVID-19 than people
who are not pregnant or recently pregnant. This includes higher
chances of being admitted to intensive care and needing to be
put on a ventilator to breathe. Some studies have also reported
a slightly higher chance of death. The chance of these outcomes
is higher among people who also have other underlying health
conditions, such as obesity, pre-pregnancy diabetes, and/or chronic
hypertension, and among those who are not fully vaccinated against
COVID-19.
c. “Having COVID-19 in pregnancy increases the chances
of having a baby before 37 weeks of pregnancy” known as
preterm delivery and stillbirth, and some studies have reported
increased chances of dangerously high blood pressure known as
“preeclampsia” and the need for emergency “c-section”.
d. “Blood clots” COVID-19 infection can increase the chance
of developing blood clots, especially if the infection is severe.
The American Society of Hematology recommends that all adults
who are hospitalized with COVID-19 be given treatment to help
prevent blood clots. Adverse pregnancy outcomes were prevalent
in COVID-19 infected females and varied by location, type, and size
of the studies. Regular screening and early detection of COVID-19 in
pregnant women may provide more favorable outcome [36].
Muscular System
How muscular system is affected:“Muscular System” permits movement of the body, maintains posture, and circulate blood throughout the body. The muscular system allows for movements by contracting, it consists of skeletal, smooth, and cardiac muscles. The muscle system in vertebrates is controlled through the nervous systems, although some muscles like the cardiac muscle can be completely autonomous. Smooth muscles are controlled directly for the autonomic nervous system and are involuntary, meaning that they incapable of being move by conscious thought, for example the heart muscles. Studies have described how SARS-CoV-2 infection induces systemic elevations of “cytokines” and signaling molecules such as “CKCL19, IFN-γ, IL-1β, IL-6, IL-8, IL-17 and TNF-α”. These inflammatory molecules have numerous potential mechanisms by which they may cause musculoskeletal symptoms [37]
Post-COVID disease on the muscular system:Early studies have indicated that there is also considerable musculoskeletal dysfunction in some patients with COVID-19. The most common post-COVID disease on the muscular system are “fatigue”, “myalgia” as a pain feeling like a pulled muscle, “arthralgia” as pain in joints, “neuropathies/myopathies” and others.
How muscular system affects others symbiotic systems:Previous studies have demonstrated that infection with the virus induces a proinflammatory state in patients with systemic effects as a result. The inflammatory response and its impact on the respiratory system have been the focus of most studies. However, “the literature is more limited regarding the inflammatory response and its implications for other organ systems, specifically the musculoskeletal system”. Previous studies have described how systemic inflammation may play a role in bone and joint pathology. Inflammation has also been linked to damage and disease of skeletal muscle.
Attention needed:Investigating the potential impact COVID-19 induced inflammation has on musculoskeletal health is essential to adequately understand and treat these symptoms.
Lymphatic System
How lymphatic system is affected:“Lymphatic system” is a network of tissues and organs that help rid the body of toxins, waste, and other unwanted materials. The primary function of the lymphatic systems is to transport lymph, as a fluid containing infection fighting white blood cells, throughout the body. The lymphatic system primary consists of vessels, which are like the circulatory system veins and capillaries. The vessels are connected to lymph nodes, where the lymph is filtered. The immune system does not develop in anatomical isolation. Its development is inherently linked to that of the lymphatic system. Furthermore, its function is synergistically linked to lymphatic activity.
Post-COVID disease on the lymphatic system:The “Pfizer-
Bio-nTech” and “Moderna” vaccines both use “lipid nanoparticles
(LNP) as mRNA carriers”, while the “Oxford Astra-Zeneca” and
“Sputnik” vaccines use “adenovirus vectors”. mRNA and viral
vaccines must transfect cells to produce their corresponding
proteins, whilst other vaccines, such as the Chinese Sinovac vaccine,
deliver inactivated virus proteins directly into muscle. Whichever
delivery system is used, viral proteins do not initiate immune
memory responses in muscles. They must be transported to lymph
nodes to initiate a response. This transport occurs primarily within
“antigen-presenting cells (APC)”, specifically “dendritic cells (DC)”,
which are drawn from blood into the vaccination site by local
inflammation. Within tissues they are activated and endocytose
and process viral proteins, expressing them in the context of surface
“major histocompatibility complex (MHC) molecules”. The critical
next step is entry into tissue-draining afferent lymphatics; this
process is actively facilitated by expression of “lymphatic-homing
molecules” on activated dendritic cells (DC). The most frequently
symptoms are [38]:
i. “Swollen lymph nodes” the lymph nodes are where the
immune system of the neck is located, so any infection in the head
or neck will cause an activation of the lymph nodes as they get
inflamed
ii. “Crisis-level hypertension” is high pressure in the arteries
generally include unexplained fatigue and headache
How lymphatic system affects others symbiotic systems:The lymphatic system is a network of lymphatic vessels, lymphoid tunnels, and organs through the body. It transports fluids from blood and houses immune cells for body defense. The lymphatic vessels pick up leaked fluid and proteins from skeletal muscle, where the muscle protect superficial lymph nodes.
Attention needed on the lymphatic system research:The muscles help lymph fluid must travel to the body up to heart, besides SARS-CoV2 entry and spread in the lymphatic drainage system of the brain [39]. With on-going research, we are now slowly appreciating “how important the lymphatic system is for generating and sustaining immune responses”. The heart of the immune system is the lymphatic system, and it is responsible for hydration throughout the body. There is not a clear understanding of how the lymphatic system operates at all [40].
Endocrine System
How endocrine system is affected:“Endocrine system” is the collection of glands of an organism that secrete hormones directly in the circulatory system to be carried towards distant target organs. The major endocrine glands include “pineal gland, adrenal, pituitary gland, pancreas, ovaries, testes, thyroid gland, hypothalamus, and adrenal glands”. Several glands that signal each other in sequence are usually referred to as an axis, for example, the “hypothalamic-pituitary-adrenal axis”.
Post-COVID disease on the endocrine system:The Post- COVID disease on the endocrine system present: “Irregular thyroid hormones”, “Anemia” as frequently a clinical condition accompanying thyroid diseases, “Subacute thyroiditis (SAT)” refers to the inflammation of the thyroid and includes a group of disorders that cause the thyroid to become inflamed. Causes pain and discomfort in the thyroid. People with this condition will also have symptoms of “hyperthyroidism” and later develop symptoms of “hypothyroidism”.
How endocrine system affects others symbiotic systems:In addition to the specialized endocrine organs, many other organs
that are part of other body systems, such as bone, kidney, liver, heart,
and reproductive glands, have secondary endocrine functions. The
COVID-19 affectations are detected frequently as:
i. “COVID-19 and endocrine pancreas” affecting more to
patients with pre-existing “type 2 diabetes mellitus (T2DM)”,
Obesity has also been found to be associated with severe disease
in COVID-19. “Adipose tissue express ACE2”, with higher adipose
tissue, more would be the overall ACE2 expression that would act
as receptors for SARS-CoV-2.
ii. “COVID-19 and adrenal gland” based on the primary
immune invasive strategy utilized by the SARS-CoV-2, like the
influenza virus, is to knock down the host’s cortisol stress response.
A remarkably interesting “hypothesis that had been proposed is the
expression of certain amino acid sequences by the SARS-CoV-2 that
are molecular mimics of the host adrenocorticotropic hormone
(ACTH)”.
iii. “COVID-19 and the hypothalamus–pituitary” based in
neurological manifestations do occur in patients with COVID-19
and include, among others, hyposmia. Expression of ACE2 by the
olfactory epithelial supporting cells could explain much of these
olfactory symptoms.
iv. “COVID-19 and thyroid” autopsy study has shown marked
destruction of the follicular and parafollicular cells of thyroid.
Destruction of follicular cells would manifest as low T3 and T4;
parafollicular cell damage would theoretically lead to low levels of
serum calcitonin.
Attention needed in the Endocrine System research:The portal of entry of the virus into the central nervous system (CNS) remains uncertain and could be via hematogenous route or directly thorough the cribriform plate. But “hypothalamic and pituitary tissues do express ACE2” and can theoretically be the viral targets. In fact, on autopsy studies, edema, and neuronal degeneration along with identification of SARS genome have been shown in the “hypothalamus”. Biochemical evidence of hypothalamus-pituitary involvement in SARS. “Endocrine manifestations in the post-acute COVID-19 setting may be consequences of direct viral injury, immunological and inflammatory damage, as well as iatrogenic complications” [41]. The possibility that “thyroid dysfunction may also increase susceptibility for COVID-19 infection deserves further investigation”. Recent data illustrate the importance of thyroid hormone in protecting the lungs from injury, including that associated with COVID-19
Integumentary System
How integumentary system is affected:“Integumentary system” that protects the body from various kind of damage, such as loss of water or abrasion as a wound caused by superficial damage to the skin, no deeper than the epidermis. The system compromises the skin including epidermis, and dermis including sweat gland, sebaceous gland (oil), hair follicle, blood vessels, nerves, nails, etc. This system has a variety of functions as: waterproof, cushion, and protect the deeper tissues, excrete wastes and regulate temperature, and is the attachment site for sensory receptors to detect pain, sensation, pressure, and temperature, besides with significant exposure to sunlight, the integumentary system also provides for vitamin D Synthesis.
Post-COVID disease on the integumentary system:The primary etiologies include “vasculitis” as group of conditions characterized by the inflammation of blood vessels that causes headache, fatigue, and fever versus direct viral involvement. There are several types of skin findings described in association with COVID-19*. These include reactions as [43] maculopapular rashes,urticaria, vesicles, petechiae, purpura, chilblains, livedo racemosa, distal limb ischemia.
Note*: While most of these dermatologic findings are selfresolving, they can help increase one’s suspicion for COVID-19.
Long post COVID symptoms report persistent skin rashes manifestations, as urticarial and morbilliform eruptions were relatively ephemeral, whereas “papulosquamous eruptions”, and particularly “pernio”, were longer-lasting.
How integumentary system affects others symbiotic systems:The tropism of the virus for the “structures of the bronchial mucosa and the immune system cells” with a typical histopathologic pattern has been demonstrated by using autopsy specimens from the lung, heart, kidney, spleen, bone marrow, liver, pancreas, stomach, intestine, thyroid, and skin [43].
Attention needed on the integumentary system:More research is needed on dermatologic manifestations of COVID-19 may be the first presenting sign of infection; so, dermatologists and doctors examining the skin should be aware of the virus’s influence on the integumentary system to promptly diagnose and treat the infected patients.
Key points observed on post-COVID research
People with post-COVID conditions may develop or continue to have symptoms that are hard to explain and manage for [44]:” clinical evaluations and results of routine health tests”, “analysis of multiorgan symptoms”, “follow-up on levels of multisystem inflammatory syndrome in multiple organs”, “post- syndromes detection and classification”, “personalized post-COVID-19 followup” and others. Where:
Clinical evaluations and results of routine health tests:Clinical evaluations and results of routine blood tests, chest x-rays, and electrocardiograms may be sometimes normal on post-COVID and presenting symptoms that are like “myalgic encephalomyelitis/ chronic fatigue syndrome (ME/CFS)”. “ME/CFS” is as a serious long-term illness that affects many body systems, and other poorly understood chronic illnesses that may occur after other infections.
Analysis of multiorgan symptoms:People who had severe COVID-19, experience multiorgan effects or autoimmune conditions with symptoms lasting weeks or months and maybe years after COVID-19 illness. Multiorgan effects can involve many body systems, including the heart, lung, kidney, skin, and brain. As a result of multiorgan effects, people that had COVID-19 are likely to develop new health conditions such as diabetes, heart conditions, or neurological conditions compared with people who have not had COVID-19.
Follow-up on levels of multisystem inflammatory syndrome in multiple organs:People who experience “multisystem inflammatory syndrome (MIS)” that can affect “children (MIS-C)” and “adults (MIS-A)”. “MIS” is a rare but serious condition associated with COVID-19 in which different body parts become inflamed, including the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal organs during or after COVID-19 illness [45].
Post-syndromes detection and identification:People experiencing any severe illness, hospitalization, or treatment may develop problems such as “post-intensive care syndrome (PICS)”, thar very hard to detect and more to identify “PICS” is a series of symptoms that people who have stayed for long in intensive care units suffer. They might experience cognitive and physical impairment, a part of mental issues due to the traumatic experience. Speak about how this situation can affect those patients with this modern template for medical purposes and help them and their families to have a better transition back to normality.
Personalized post-COVID-19 follow-up:The estimates for how many people experience post-COVID conditions can be quite different depending on who was included in the study, as well as how and when the study collected information. Estimates of the proportion of people who had COVID-19 that go on to experience post-COVID conditions can vary: 13.3% at one month or longer after infection, 2.5% at three months or longer based on selfreporting and more than 30% at 6 months among patients who were hospitalized. The research must be re-organized accordingly to the post-COVID clinical manifestations in multiorgan including follow-up studies.
How Organizing by Categories for the Research for COVID/Post-COVID
“Post COVID-19” is characterized by persistent COVID-19 symptomatology that lasts for, at least, two months. The typical symptoms as fatigue, cough, or dyspnea, in some old people coexist unspecific symptoms as functional deterioration, cognitive impairment, or delirium that could apparently mitigate the prevalence of this syndrome in this age group. Its main consequence is the functional decline, leading to a development of “sarcopenia” as loss of muscle tissue as a natural part of the aging process, frailty, and disability, without forgetting the nutritional and cognitive disorders [46]. The “post COVID symptoms from clinical manifestations” research must be re-organized by at least 4 categories [47]: “by previous COVID infection”, “by COVID treatment and hospitalization”, “COVID infection damage or by the real post-COVID syndrome”, and “trigger after COVID infection”. Their descriptions of these “post COVID symptoms from clinical manifestations” and examples that are explained in the following sections.
By Previous COVID Infection
These are previous COVID infection pathological condition as
“sequels of a pathological condition resulting from a prior disease,
injury, or attack and/or by consequence has an organ damage
following for acute disease”. It is important to notice that the
present pathology could be or not post-infectious disease since it is
related to a previous organ damage the most frequent are:
a. “Thrombotic” as formation or presence of blood
clots within a blood vessel or “cardiac” altering the “symbiotic
cardiovascular or circulatory system”.
b. “Psychiatric” or “neurological” affecting the “symbiotic
nervous system”.
c. “Pulmonary” affecting the “symbiotic respiratory system”.
d. “Renal” altering the “symbiotic excretory system”.
e. “Sexual” affecting the “symbiotic reproductive system”.
And many others
By COVID Treatment and Hospitalization
These pathology conditions are derived from the hospitalization
itself, and which would be common with other behaviors as:
a. “Post-Intensive Care Unit (ICU) syndrome” a group of
neuropsychiatric disorders that limit the functioning of patients
after a prolonged hospitalization in ICU including anxiety,
depression, post- traumatic stress disorder, motor weakness
altering the “symbiotic nervous system”.
b. “Secondary to a prolonged hospitalization” as motor
weakness altering “symbiotic muscular system”.
c. “Isolation measures and/or the restriction of visits being
in the hospital” as fatigue, cognitive or psychiatric disorders by
altering the “symbiotic nervous system”.
d. “Decompensation of a previous chronic diseases” this
is for avoiding mixing too many medicaments during the COVID
treatments in the hospital, with the ones that the patient is
currently taking as the ones needed for: “heart disease”, “cancer”,
“chronic lung disease”, “stroke”, “Alzheimer disease”, “diabetes”,
“chronic kidney disease”, “chronic liver disease” and many others.
e. “Pharmacological toxicity” by the effects of treatments
administered during hospitalization. It is the toxicity due to
interaction of the drug with the same target that produces the
desired pharmacological response. The concept is not one of
competitive inhibition but rather that the biological response that
the drug exhibits upon binding to its target is the same one that
produces both the efficacious and the toxic effect
f. Others similar.
COVID Infection Damage or by the Real Post-COVID Syndrome
These are clinical manifestation different from anterior categories that persist over time after COVID that would constitute the “real post-COVID syndrome” as a post-infectious syndrome per se.
The most frequently symptomology reported by WHO and CDC
as the following examples describe [48]:
a. “Vasculitis” as inflammation that can affect very small
vessels, medium-size blood vessels, or large blood vessels such
as the “aorta” in the heart. Some research has shown blood vessel
damage and
inflammation referred to as “vasculitis in COVID-19 patients’
brains and central nervous system (CNS)”. Infection with severe
acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been
associated with several neurologic manifestations including the
development of cerebral lesions
resembling “CNS vasculitis” in elderly patients with severe
coronavirus disease 2019 (COVID-19) [49].
b. “General symptoms as tiredness or fatigue” that interferes
with daily life. These symptoms get
worse after physical or mental effort or inclusive “postexertional
malaise” that is not always related to an underlying
condition and may be caused by stress, fear, inadequate sleep, and
fever.
c. “Respiratory and heart symptoms” when there is a
difficulty on breathing or shortness of breath, cough, chest pain,
and heart palpitations.
d. “Neurological symptoms” as “brain fog” presenting
difficulty thinking or concentrating, headache, sleep problems,
dizziness when you stand up (lightheadedness), pins-and-needles
feelings, change in smell or taste, depression, or anxiety.
e. “Digestive symptoms” as diarrhea, stomach pain, etc.
f. Other symptoms as joint or muscle pain, rash, changes in
menstrual cycles, etc.
Trigger After COVID Infection
The COVID-19 infection could act as a trigger for other disease
as:
a. “Autoimmune” altering the “symbiotic immune and others
organs in different symbyotic systems”
b. “Metabolic disease” as:
i. Diabetes affecting the “symbiotic digestive system”, and
others organs in different symbyotic systems.
ii. Hypothyroidism and hyperthyroidism affecting the
thyroid in the “symbiotic endocrine system”.
c. “Recombinant” as the process in which the genomes
of two SARS-CoV-2 variants or the possibility of one SARS-CoV-2
variant with others kind of virus that have infected a person at the
same time combine during the viral replication process to form a
new variant that is different from both parents’ lineages.
d. “Inexplicable symptoms that are similar to myalgic
encephalomyelitis/chronic fatigue syndrome (ME/CFS)”, when
clinical evaluations and results of routine blood tests, chest
x-rays, and electrocardiograms may be normal, and the pathology
condition is similar to “ME/CFS”
e. “Multisystem inflammatory syndrome (MIS)” that can
affect “children (MIS-C)” and “adults (MIS-A)”. illness”. Where:
“multiorgan effects” can involve many body systems, including the
heart, lung, kidney, skin, brain, and other organs. And others similar
COVID/Post COVID Management Based on Multiorgan Multidisciplinary Systems
Some of the most frequent proposed management for “long
COVID-19” are [50]:
a. “Respiratory System” evaluated with a clinical assessment,
pulmonary function test, chest X-rays*.
i. *Usually applied to all patients at 12 weeks after COVID-19,
when an abnormal chest X-ray and /or clinical impairment has been
observed and a further higher resolution “Computer Tomography
(CT)” is recommended.
b. “Cardiovascular or circulatory system” evaluated
with a details clinical examination, non-invasive assessment,
electrocardiogram, echocardiography, CT or “Cardiovascular
magnetic resonance imaging (CMR)” for patients with suspected
pulmonary embolism, blood analysis, venipuncture, duplex
ultrasound, for lower climb clots, computed tomography
angiography.
c. “Nervous system” with screening strategy used to look for
as-yet-unrecognized conditions or risk marker for stress, anxiety,
depression, besides CT scan, electroencephalogram, MRI.
d. “Excretory system” as urine analysis, glomerular filtration
rate, CT, CTA, MRI.
e. “Endocrine system”: with medical images from “magnetic
resonance cholangiopancreatography” as an examination of the
bile and pancreatic ducts with contrast medium. And many other
managements are needed to cover the other symbiotic systems.
“Post COVID-19 symptoms analysis” really needs others many others clinical assessments, medical and cognitive tests, imaging, mew techniques combined with lab analysis from different organs to find the real reasons of the connection between them, to take appropriate measurements to detect, follow-up, and prevent post-COVID symptoms as: “fatigue”, “smell loss”, “alteration on epigenetic age”, “cognitive decline”, “infected immune cells and massive inflammatory response”, “neuropathy”, “brain infection”, and others.
Fatigue
“Fatigue” can be trigger for many functions as neuroendocrine,
autonomic, and immune dysfunction, cognitive dysfunction,
post-exertional malaise (PEM) as an important part of chronic
fatigue syndrome (ME/CFS) to discover what triggers, symptom
consequences, features, duration, and latency*. Besides:
a. “Anaerobic capacity study” as the maximal amount of
“adenosine triphosphate resynthesized via anaerobic metabolism”
by the whole organism during a specific mode of short-duration
maximal exercise, to know the ability to produce energy without
oxygen.
b. “Pneumotachograph and gas analyzers” to know diffusing
capacity for lung carbon monoxide.
c. “Spirometry” as a group of tests that assess how well the
lungs work by measuring lung volume, capacity, rates of flow, and
gas exchange.
Note*: COVID-19 has impacted sleep and mental health, researchers found that stress, anxiety, and depression besides could also be a reason for fatigue [51].
Smell Loss
Researchers have discovered a mechanism that may explain why COVID-19 patients lose their sense of smell; the presence of the virus near neurons in the “olfactory tissue” brought an inrushing of “immune cells, microglia, and T cells”, that sense and counter infection. Such cells release proteins called “cytokines” that changed the genetic activity of olfactory nerve cells, even though the virus cannot infect them. In most cases, the smell loss lasts only a few weeks, but for more than 12 percent of COVID-19 patients, olfactory dysfunction persists in the form of ongoing reduction in the ability to smell identified as “hyposmia” or changes in how a person perceives the same smell known as “parosmia”.
Experiments confirmed that SARS-CoV-2 infection, and the immune reaction to it, decreases the ability of DNA chains in chromosomes that influence the formation of olfactory receptor building to be open and active, and to loop around to activate gene expression. In both hamster and human olfactory neuronal tissue, the research team detected persistent and widespread downregulation of olfactory receptor building [52].
Alteration on Epigenetic AgeThe “epigenetic age” reflects the biological events that lead to aging. It is similar but not identical to the “chronological age”. When it moves faster it is an indication of faster aging and when it moves slower aging is slowed down. Epigenetic ages of everyone are determined by applying epigenetic clocks and telomere length estimator to the methylation profile of the individual. “Epigenetic age acceleration” is calculated and compared between groups.
The epigenetic age could be altered in viral infection. DNA methylation of the blood samples from healthy individuals and COVID-19 patients are profiled using “EPIC methylation array” that is a commonly used for high-throughput DNA methylation profiling [53].
Cognitive Decline
There have been reports of negative cognitive outcomes during and after SARS-CoV-2 infection, but the long-term effect of COVID-19 on cognitive function remains unclear. Six months following COVID-19 infection, two-thirds of patients still experienced “neurological symptoms” including headaches, memory impairment, and decreased concentration that impacted their quality of life.
a. Some research authors report that survivors of
COVID-19 had lower cognitive scores at both time points, and
that the “incidence of mild cognitive impairment or dementia”,
“age acceleration”, “COVID-19 Pneumonia Increases Dementia
Risk”, “cognitive alterations and brain shrinkage”, “Affectation on
attention, reasoning and problem-solving”, and many others*.
Where:
b. “Incidences of dementia and mild cognitive impairment”,
when the effects have been stronger for those who experienced a
severe form of the disease and can take patients to dementia [54].
These findings suggest that, over the long term, severe COVID-19
may lead to an increase in cognitive decline and dementia in older
adults and point to the need to evaluate the effect of the COVID-19
pandemic on future dementia burden worldwide.
c. “Lasting cognitive impairment “- typical 60% of 400
coronavirus survivors experienced, a cognitive problem in those
who experienced mild-to-moderate COVID symptoms, as well as
those who experienced more severe symptoms. One in three of
the survivors experienced severe cognitive symptoms, akin to
dementia [55].
d. “Age acceleration” researchers found that cognitive
impairment from severe COVID-19 equivalent to 20 Years of Aging
[56]. Many people out there still experiencing problems with
cognition many months later. We urgently need to look at what can
be done to help these people.
e. “COVID-19 Pneumonia Increases Dementia Risk” patients
hospitalized for COVID-19 associated pneumonia had an increased
risk of developing dementia compared to patients hospitalized
for other forms of pneumonia. The median time interval between
infection and dementia diagnosis was 182 days for COVID-19
patients. The study only included new onset dementia associated
with hospital admission during a short follow-up period [57].
f. “Cognitive alterations and brain shrinkage” even mild
COVID-19 infection can lead to cognitive alterations and brain
shrinkage, researchers report that COVID can affect the brain has
come from studies of severe infection. In people with severe COVID,
inflammatory cells from outside the brain can enter brain tissue and
spread inflammation. There may be changes to blood vessels, where
the brain cells can even have changes like those seen in people with
decrease in brain volume that are common to many brain diseases
and disorders associated with degeneration and have been found
in people with mild cognitive impairment, Alzheimer’s disease,
depression, and traumatic brain injury, among others [58,59].
g. “Affectation on attention, reasoning and problem-solving”
problems in thinking and attention linked to COVID-19 Infection.
Those with more server COVID symptoms fared worse on cognitive
tests, specifically associated with reasoning and problem-solving.
“Going forward it would be valuable to bring together brain imaging
and cognitive tests with other information on mental health and
everyday function, ideally in studies that track peoples’ trajectories
for months or even years”. To really know what the long-term effects
are for people will require people to be followed up over time” [60].
And many other authors report that survivors of COVID-19 had
lower cognitive scores.
*“People’s cognition and quality of life still impacted so long after infection is something we need to be taking a serious look at. It is imperative to know how common this is, what biological processes are causing this, and what ongoing health care these people will need. This work is an important first step to getting there” [61].
*Fortunately, there is evidence that a solution is helping on improves Cognitive deficits as in Long-COVID improve cognitive applying “Brain Stimulation”. The good news is that Cognitive deficits because of long-COVID can be significantly improved within 3-4 days following alternating using non-invasive brain stimulation using microcurrents [62]. Many recovered COVID-19 patients continue to exhibit significant and long-lasting cognitive deficits in memory, attention, language comprehension and multitasking, as well as fatigue. These symptoms can persist for many weeks to months after the early symptoms of infection have subsided.
Infected Immune Cells and Massive Inflammatory Response
Some studies have found that immune cells infected with SARSCoV- 2 can trigger a “massive inflammatory response that could cause severe COVID-19*” [63,64]. They found that two types of white blood cells “macrophages” in the lungs, and “monocytes” in the blood which, once infected with the virus, trigger the inflammation. The studies also provide conclusive evidence that the virus can infect and replicate in immune cells and reveal how it enters those cells. Evidence of such infections has been mixed until now. Both during and after infection with the Coronavirus SARS-CoV-2, patients may suffer from severe neurological symptoms, including “anosmia (loss of smell)”, the loss of taste and smell typically associated with COVID-19. Along with direct damage caused by the virus, researchers suspect a role of excessive inflammatory responses in the disease.
There is already evidence of “central nervous system (CNS)” involvement in COVID-19, the extent of inflammation in the brain the many “microglial nodules”. Using a novel measurement method, “imaging mass cytometry”, they were able to determine different cell types as well as virus-infected cells and their spatial interaction in previously unseen detail [65]. Many reports hold that “unregulated NLRP3 inflammasome activation” may potentially contribute to the severity of COVID-19 and its aftermath. It is therefore possible that suppression of “NLRP3” as a protein that in humans that is encoded by the NLRP3 gene located on the long arm of chromosome.
*This inflammasome activity as a protein complex in the cytoplasm of a cell that regulates immune and inflammatory responses to pathogens may prove efficacious against both acute lung disease and chronic neurological after-effects.
*Potential Therapeutic Use of the “Rosemary Diterpene Carnosic Acid” for Alzheimer’s Disease, Parkinson’s Disease, and Long-COVID through NRF2 Activation to Counteract the NLRP3 Inflammasome [66].
Pain and Neuropathy
A significant number of people suffering from long COVID experience sensory abnormalities, including various forms of pain, tingling sensations, and numbness in hands and feet. Now on the following research they report about evidence as: “COVID-19 infection could cause pain”, “COVID-19 can damage nerves”, and “COVID-19 can cause neuropathy “.
a. “COVID-19 infection could cause pain” and leaves evidence in a gene expression signature related with pain in the “dorsal root ganglia” which persists after the virus has cleared. A “dorsal root ganglion” is a cluster of neurons in a dorsal root of a spinal nerve. The cell bodies of sensory neurons known as first-order neurons are in the “dorsal root ganglia”. The signature matched other gene expression patterns seen in pain caused by other conditions [67]. b. “COVID-19 could damage nerves” several viral infections as “HIV” and “shingles” are associated with peripheral neuropathy because “viruses can damage nerves”. It is important to understand whether a viral infection is associated with an increased risk of neuropathy. There is no established diagnosis of neuropathy related to COVID-19, current treatments for neuropathy are somewhat similar. Pain specialists use the same types of medications to treat peripheral neuropathy, whether it’s caused by “diabetes” or “HIV”, the cause is unclear [68]. c. “Evidence of neuropathy cause by COVID” several patients who contracted COVID-19 in the early months of the pandemic reported symptoms of neuropathy that is a group of diseases resulting from damaged or malfunctioning of nerves that causes weakness, numbness and pain in hands and fee that lasted up to three months after recovery. There is evidence on this research nearly 30% of patients who tested positive for COVID-19 also reported neuropathy problems at the time of their diagnosis, and that for 6% to 7% of them, the symptoms persisted for at least two weeks, and up to three months, suggesting this virus may have lingering effects on peripheral nerves [69].
Brain Infection
“COVID-19 affects central nervous system and brain”, “COVID-19
triggers immune response in brain”, “Genetic link between risk
for Alzheimer’s disease and severe COVID-19”, “COVID-19 makes
molecular changes”, “Persistent lack of smell is associated with
brain changes”, “Assembloids shows how COVID-19 infects brain
cells”, “COVID-19 protein Interacts with Parkinson’s Protein”,
“Probably potential correlation between COVID infection and
microbiome disturbance”
a. “COVID-19 affects central nervous system and brain”
studies reveal, in detail, how COVID-19 infection affects the “central
nervous system”, including inducing “brain injury and inflammation
consistent with reduced cerebral blood flow” [70]. Where severe
brain inflammation and injury consistent with reduced blood flow
or oxygen to the brain, including neuron damage and death. They
also found small bleeds in the brain. Surprisingly, these findings
were present in subjects that did not experience severe respiratory
disease from the virus. The findings are also consistent with
autopsy studies of people who have died of COVID-19, suggesting
that nonhuman primates may serve as an appropriate model, or
proxy, for how humans experience the disease.
b. “COVID-19 triggers immune response in brain” study
reveals how COVID-19’s spike protein has a similar effect on the
brain’s immune cells as it does throughout the rest of the body [71].
The big question is: “If the spike protein used by the coronavirus to
enter human cells can have a similar effect on the brain’s immune
cells as it does with the rest of the body, then could be possible
that the coronavirus that has affected the brain pose a high risk for
neurodegenerative disorders further down the line, like Alzheimer’s
or Parkinson’s?”
c. “Genetic link between risk for Alzheimer’s disease and
severe COVID-19” An anti-viral gene that impacts the risk of both
Alzheimer’s disease and severe Covid-19 has been identified by
a UCL-led research team [72]. The researchers estimate that one
genetic variant of the OAS1 gene increases the risk of Alzheimer’s
disease by about 3-6% in the population, while related variants on
the same gene increase the likelihood of severe Covid-19 outcomes.
The findings, published in Brain, could open the door for new
targets for drug development or tracking disease progression in
either disease, or suggest that treatments developed could be used
for both conditions. The findings also have potential benefits for
other related infectious conditions and dementias.
d. “COVID-19 makes molecular changes” inside neurons,
defective ryanodine receptors have previously been linked to
an increase in “phosphorylated tau”, a well-known hallmark of
“Alzheimer’s”. In the new study, the Columbia researchers found
high levels of phosphorylated tau in the brains of the COVID patients
in addition to defective ryanodine receptors [73].
e. “Persistent lack of smell is associated with brain changes”
once the virus has affected the olfactory bulb and caused effects
there are changes that we can see with imaging then other places
in the brain that are connected to it also become abnormal, either
in function or structure or both [74]. The olfactory bulb has
connections to regions of the temporal lobe. We often talk about
the temporal lobe in the context of aging and Alzheimer’s disease
because it is where the hippocampus is located. The hippocampus
is likely to play a key role in aging, given its involvement in memory
and cognitive processes.
f. “Assembloids shows how COVID-19 infects brain cells”
neuroscientists and infectious disease specialists, confirmed that
human neural cells are resistant to SARS-CoV-2 infection. However,
recent studies hinted those other types of brain cells might serve as
a “Trojan horse”. For example, “Pericytes” are specialized cells that
wrap around blood vessels and carry the SARS-CoV2 receptor. The
researchers introduced “pericytes” into three-dimensional neural
cell cultures known as brain organoids to create “assembloids”, a
more sophisticated stem cell model of the human body [75]. These
“assembloids” contained many types of brain cells in addition to
“pericytes” and showed robust infection by SARS-CoV-2. Their
results indicate that one potential route of SARS-CoV-2 into the
brain is through the blood vessels, where SARS-CoV-2 can infect
“pericytes”, and then SARS-CoV-2 can spread to other types of brain
cells. Alternatively, the infected pericytes could lead to inflammation
of the blood vessels, followed by clotting, stroke or hemorrhages,
complications that are observed in many patients with SARS-CoV-2
who are hospitalized in intensive care units [76].
g. “COVID-19 protein Interacts with Parkinson’s Protein”
and promotes “amyloid Formation”. The COVID causing SARS-CoV-2
protein interacts with alpha-synuclein, speeding up the formation
of amyloid plaques. “Amyloid” is linked to cognitive decline in
patients with Parkinson disease without dementia [77,78].
h. “Probably potential correlation between COVID infection
and microbiome disturbance” microbiome is a collective genome
of the microbes composed of bacteria, fungi, protozoa, and viruses,
which live inside and on the human body, but primarily in the
human gut. The gut microbiota is thought to be key mediators in the
bi-directional communication between the gut and the brain along
the gut–brain axis that influence neurodevelopment, brain function,
and behavior an undesirable shift in microbiota composition,
termed dysbiosis, has been associated with metabolic diseases
such as inflammatory bowel disease, obesity, and diabetes. The gut
microbiome and the brain communicate with each other through
neural, inflammatory, and hormonal signaling pathways. As a result
of the two-way interaction between the gut microbiome and the
brain, each can send messages that impact the other. Studies have
shed light on the potential correlation between COVID infection and
microbiome disturbance but have limitations that require further
investigations with larger sample sizes to approximate the general
population [79].
All this information on COVID-19/post-COVID-19 and the results are complicated to process, relate them, and obtain conclusions is a huge work to do, due to the enormous size and variety of specialized data involved, where is so important and critical to keep a valid tracking of all of them, especially at the followup, and pre-diagnostic as well other deductions as forecasting. Then the need for “Artificial Intelligence” solutions must be applied under a “multidisciplinary healthcare specialized cloud computer framework*” to cover all the needs for multiple-organ diagnostics and necessary tests obtained from local health equipment as image and special diagnostic this is a necessity now specially for the cognitive analysis and others for post-covid symptoms.
*One powerfully example has been proposed and explained at the book/eBook Applied: “Biomedical Engineering Using Artificial Intelligence and Cognitive Model” as described on chapter 7 “Cognitive learning and reasoning models applied to biomedical engineering” [80] and it is introduced in the next two section.
Artificial Intelligence Applied for COVID/post- COVID Analysis
A multidisciplinary health analysis using for detection, followup, progression analysis, and even prediction of COVID-19 and post-Covid is urgently needed using as a complete solution under specialized software and powerful specialized hardware introduce in the next section. Specialized software applying powerfully and well design “Artificial intelligence algorithms”, that includes “Machine Learning”, “Deep learning” and “Cognitive Learning” also known as “cognitive computing” [81]. Where:
Artificial intelligence
“Artificial intelligence (AI)” is an area of “computer science” that emphasizes the creation of intelligent algorithms running machines that work and react like humans [82]. “Machine Learning (ML)” is a subset of “AI,” and it defined as the scientific study of algorithms and statistical models that computer systems use to perform a specific task effectively without having to use explicit instructions, relying on patterns and inference [83]. “Deep Learning (DL)” is a subset of “ML,” and it is defined as the algorithms inspired by the structure and function of the “human brain,” such as the “Artificial Neural Networks (ANN)” that are designed to recognize patterns that are represented by numeric vectors that represent images, sound, text, or time series [18, 84].
“Cognitive Computing (CC) or Cognitive Learning (CL)” are special applications that are implemented using any combination of “AI” technologies to build “cognitive models” that “mimic human thought” processes using “speech and vocalization under Natural Language Process (NLP),” “handwriting recognition,” “face identification and their specific movements,” “behavioral pattern determination” and other special algorithms, such as “sentiment analysis”. “Cognitive Learning” is used to assist humans in their decision-making process and in this book [85] are proposed as methods to evaluate “human cognitive status.”
Examples of Evaluating Human Cognitive Status with AI
Cognitive learning is a subset of AI that can deduct if the
learning in human is correct based on his answers and compare
them to analyze the human cognition status, are [22,86]: “deductive
reasoning”, “deductive reasoning,” “inductive reasoning,” “abductive
reasoning,” “metaphoric reasoning,” “neuro-fuzzy logic reasoning,”
“visuospatial relational reasoning,” and others. Where:
a. “Deductive reasoning” is the process of drawing
conclusions that are guaranteed to follow from given premises.
There are many types of “deductive reasoning”, they are an
essential element of “cognitive development and human thinking”
based on relation of effect, applying categories to identify them and
propositions between facts.
b. “Inductive reasoning” is when the premises show
evidence for a general possible truth. It is the opposite of “Deductive
reasoning”. “Psychological research” has found that “inductive
reasoning tests” are highly valid measures of a “person’s cognitive
ability”.
c. “Abductive reasoning” typically begins with a possible
incomplete set of observations and proceeds to the likeliest possible
explanation for the set, that is, “a medical diagnosis given this set of
symptoms, where the diagnosis would best explain most of them”.
“Abductive reasoning” is the logical process where one chooses a
hypothesis that would best fit the given facts.
d. “Metaphoric reasoning” is defined as the cognitive act
that enables a description of an object or event, real or imagined,
using concepts that cannot be applied to the object or event
in a conventional way. “Metaphoric reasoning” is a linguistic
manifestation of a “cognitive process” based on “analogical
reasoning“.
e. “Neuro-fuzzy logic reasoning” is based on “Fuzzy logic
reasoning”, which “resembles human reasoning in a like on way
how humans perform decision-making”. it involves all intermediate
possibilities between “YES” and “NO”.
f. “Visuospatial relational reasoning” reasoning” is a kind
of “relational reasoning” using images for reasoning. It investigates
the relational reasoning using visuospatial materials with
biomedical images as the functional magnetic resonance imaging.
“Neurology applying Artificial Intelligence to evaluate the human
cognitive processes through cognitive computing” and because of
the analysis of learning, reasoning, and others, the correlation of
biological processes with brain activity can be studies using imaging
techniques. “Visuospatial relational reasoning” is a method that
has indicated how the “human brain” is involved simultaneously in
many activities at any moment in time. Any many other types of
cognitive learning.
In summary, “Cognitive Learning” is a mental process that takes in, interprets, stores, and retrieves information heard, text and images received to infer something, and can be studied by the “neuroscience of reasoning” that scientifically involves determining the neural correlates all the neurons involved as a pathway for reasoning. “Cognitive Learning” involves application develops as “Machine Learning”, “Deep learning” and all “AI algorithms” that can help in this study.
The COVID-19/post-Covid_19 research must involve a multidisciplinary health analysis that must be organized on a “multidisciplinary healthcare specialized cloud computer framework” that involved all the needs that until today is handle only by separated medical specialties. In the next section I introduce an example of that kind of smart virtual machine that is explained with al details on my book/eBook: “Applied Biomedical engineering Using Artificial Intelligence and Cognitive Model” [85].
General Architecture Framework for Multidisciplinary Health Analysis
General Architecture of a “framework of a Cognitive Computing Agents System for multidisciplinary healthcare analysis” for patients follow-up, analysis, detection, and evolution of COVID-19 and post-Covid symptoms, this system has been popularized under the name of “Health/Cognitive Cloud Computing” [86], Basically, it a configurable clouding computer where local inputs are health data from the patient status, and delivering outputs to health personnel to detect all “motor symptoms as physical disorder movements”, and “non- motors symptoms that are analyzed applying cognitive reasoning algorithms”.
The “General Architecture framework for multidisciplinary
health analysis” system also known as “Health/Cognitive Cloud
Computing” that organizes and process all information under a
new concept: “Personalized health for medical precision (PHMP)”
that will allow detection, follow-up, progression analysis, and even
prediction under two processing types: “traditional” and “PHMP”.
a. The “traditional processing” all data is compared with
other patients to define a health range calculated applying general
statistics and “AI”, and
b. “Personalized health for medical precision or PHMP”
where all information is analyzed individually, only with all the
information of each patient dataset using “Auto configurable AI
database” for the COVID-19 patients including genetic data.
The “General Architecture framework for multidisciplinary health analysis” including the “traditional” and the “Personalized health for medical precision” also known as “Health/Cognitive Cloud Computing” is shown at Figure 2. This healthcare specialized system allows to keep track and synchronized all data and results for this urgent global “COVID-19/post-COVID-19 pandemic” that started in 2019 and created major disruptions around the world demonstrated the imperative need for quick, inexpensive, accessible, and reliable diagnostic methods that would allow the detection of COVID/Post-Covid symptoms including as explained in this paper (Figure 2).
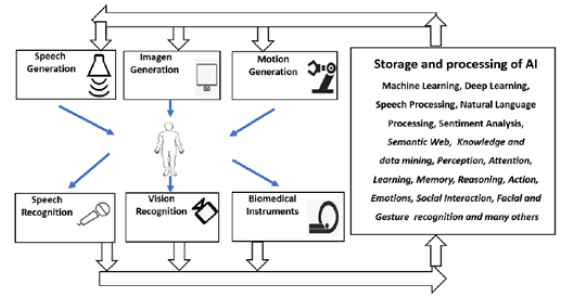
Figure 2: General Architecture framework for multidisciplinary health analysis also known as “Health/Cognitive Cloud Computing” using for follow-up, analysis, detection, and prediction of COVID-19 and post-Covid that organizes and process all information under a new concept: “Personalized health for medical precision (PHMP)*”.
Note*: More information with examples is explained in the book/eBook: “Applied Biomedical engineering Using Artificial Intelligence and Cognitive Model” [85].
Different methods and techniques with examples have been explained and developed in many research examples through this book for the components of General Architecture framework for multidisciplinary health analysis also known as “Health/Cognitive Cloud Computing” using “Cognitive Computing Agents System (AICCAS)” for: “speech recognition,” “visual recognition,” “biomedical instruments (bio instruments),” “AI dataset obtainment for biomedical engineering including cognitive detection human-like abilities,” “AI technologies evolutions as cognitive computing,” “AI models obtainment including cognitive models,” “AI human functionalities analysis including cognitive evaluations,” “inference engine,” “actions generation,” “speech generation,” “imagen generation,” and “motion generation,” and others.
Conclusions
The coronavirus pandemic has created a mass-disabling event known as “post-COVID-19 syndrome or long haulers COVID-19 or long COVID-19”, that experts comparted to “HIV”, “polio” or “World War II, with millions suffering the long-term effects of infection with the virus. Many have found their lives dramatically changed and are grappling with what it means to be disabled. “Long COVID-19 has generated a different and important face on the whole problem of long-term care,” and acted on multidisciplinary research is now a priority [87]. The big danger might come when the variant will be completely different. Each infection may bring with it the possibility of long Covid, the constellation of symptoms that can persist for months or years. It’s too early to know how often an Omicron infection leads to long Covid, especially in vaccinated people. The COVID-19 pandemic has tested our psychological limits. Some have been more affected than others by the stress of potential illness and the confusion of constantly changing health information and new restrictions. A new study finds the pandemic may have also impaired people’s cognitive abilities and altered risk perception, at a time when making the right health choices is critically important [88].
This research paper has the goal to concentrate important information to summarize discovers, treatments, classification, methods, and proposed techniques of many medical specialized doctors, health personnel and researchers around the word to help on the fast adaptation on the fighting of this virus. The main objective to help on the reorganization for the “COVID-19/long COVID-19 research analyzing with multidiscipline care using Artificial intelligence (AI) under a revolutionary mainframe” that can organize and follow-up under a new concept: “Personalized healthcare for medical precision (PHMP)” that will allow detection, follow-up, progression analysis, and even prediction under two processing types: “traditional” and “PHMP”. In the “traditional processing” all data is compared with other patients to define a health range calculated applying general statistics and on “PHMP” is analyzed only with all the information of one patient and his datasets using “intelligent and configurable database” of the COVID-19 patients including genetic data.
Notices: Knowledge and best practice in this field are constantly changing as new research and experience broaden our understanding, changes in research methods, professional practices, or medical treatment may become necessary. To the fullest extent of the law, neither the Publisher nor the authors, contributors, or editors, assume any liability for any injury and/or damage to persons or property as a matter of products liability, negligence or otherwise, or from any use or operation of any methods, products, instructions, or ideas contained in the material herein.
References
- (2022) COVID-19 Genomic Epidemiology Toolkit. Advanced Molecular Detection (AMD). CDC.
- Priya Sharma, Sumit Bharti, Isha Garg (2021) Post COVID fatigue: Can we really ignore it?, Indian J Tuberc 69(2): 238-241.
- https://www.ama-assn.org/delivering-care/public-health/what-long-covid.
- Benjamin W Neuman, Gabriella Kiss, Andreas H Kunding, David Bhellai M, Fazil Baksh, et al. (2022) A structural analysis of M protein in coronavirus assembly and morphology. Journal of Structural Biology 174(11): 11-22.
- Yongwu Hu, Jie Wen, Lin Tang, Haijun Zhang, Xiaowei Zhang, et al. (2003) The M Protein of SARS-CoV: Basic Structural and Immunological Properties. Genomics Proteomics Bioinformatics 1(2): 118-130.
- Zhihua Bai, Ying Cao, Wenjun Liu, Jing Li (2021) The SARS-CoV-2 Nucleocapsid Protein and Its Role in Viral Structure, Biological Functions, and a Potential Target for Drug or Vaccine Mitigation. Viruses 13(6): 1115.
- https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html.
- Shahhossein Nariman, Babuadze George, Wong, Gary, Kobinger Gary P (2021) Mutation Signatures and In Silico Docking of Novel SARS-CoV-2 Variants of Concern. Microorganisms 9(5): 926.
- https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html.
- https://www.cdc.gov/coronavirus/2019-ncov/variants/about-variants.html.
- https://www.nature.com/articles/d41586-022-01240-x, 06/17/2022.
- McFadyen JD, Stevens H, Peter K (2020) The Emerging Threat of (Micro)Thrombosis in COVID-19 and Its Therapeutic Implications. Circ Res 127(4): 571-587.
- https://covariants.org/.
- https://nextstrain.org/.
- Cristina Roldán Jiménez, Antonio I Cuesta Vargas (2022) Proposal for assessment of the predominant symptom and physical function in patients suffering from Long COVID. Medical Hypotheses 162: 110811.
- Garza Ulloa Jorge (2021) Why COVID-19 Long Haulers?
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/what-coronavirus-does-to-the-lungs.
- Jorge Garza Ulloa (2022) Chapter 6-Deep Learning Models Evolution Applied to Biomedical Engineering. Applied Biomedical Engineering Using Artificial Intelligence and Cognitive Models. Academic Press pp. 509-607.
- Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Napoli RD (2020) Features, evaluation,and treatment coronavirus (COVID-19).
- I W, Moore MJ, Vasilieva N, Sui J, Wong SK, et al. (2003) Angiotensin-convertingenzyme 2 is a functional receptor for the SARS coronavirus. Nature 426(6965): 450-454.
- (2022) Heart Problems after COVID-19. Johns Hopkins Medicine, USA.
- Jorge Garza Ulloa (2018) Chapter 2-Introduction to human neuromusculoskeletal systems. Applied Biomechatronics using Mathematical Models. Academic Press Pp. 53-118.
- RS Soumya, T Govindan Unni, KG Raghu (2020) Impact of COVID-19 on theCardiovascular System: A Review of Available Reports, Cardiovasc Drugs Ther 14: 1-15.
- Igor J Koralnik, Kenneth L Tyler (2020) COVID ‐19: a global threat to the nervous system. Annals of Neurology 88(1): 1-11.
- J Monserrat Sanz, AM Gómez Lahoz, R Oliva Martín (2021) Role of the immune system in SARS-CoV-2 infection: immunopathology of COVID-19. Medicine 13(33): 1917-1931.
- https://medicine.yale.edu/news-article/understanding-immune-system-blunders-in-response-to-the-coronavirus.
- https://www.sciencedaily.com/releases/2021/10/211028125803.htm.
- Song Y, Liu P, Shi XL, Chu YL, J Zhang, et al. (2020) SARS-CoV-2 induced diarrhea as onset symptom inpatient with COVID-19. Gut 69(6): 1143-1144.
- https://www.thelancet.com/journals/langas/article/PIIS2468-1253(21)00076.
- https://www.medicalnewstoday.com/articles/gastrointestinal-symptoms-in-covid-19-what-do-we-know-so-far#GI-symptoms-associated-with-COVID-19.
- https://www.webmd.com/lung/covid19-digestive-symptoms#1,6/18/2022.
- (2022) Coronavirus: Kidney Damage Caused by COVID-19. Johns Hopkins Medicine, USA.
- Joshua D Long, Ian Strohbehn, Rani Sawtell, Roby Bhattacharyya, Meghan E SISE, et al. (2022) COVID-19 Survival and its impact on chronic kidney disease. Translational Research 241: 70-82
- Megan McCool Myers, Debra Kozlowski, Valerie Jean, Sarah Cordes, Heather Gold, et al. (2022) The COVID-19 pandemic's impact on sexual and reproductive health in Georgia, USA: An exploration of behaviors, contraceptive care, and partner abuse. Contraception.
- https://mothertobaby.org/fact-sheets/covid-19/.
- Pallavi Dubey, Sireesha Y Reddy, Sharron Manuel, Alok K Dwivedi (2020) Maternal and neonatal characteristics and outcomes among COVID-19 infected women: An updated systematic review and meta-analysis. European Journal of Obstetrics & Gynecology and Reproductive Biology 252: 490-501.
- Laith K Hasan, Brittney Deadwiler, Aryan Haratian, Ioanna K Bolia, Alexander E Weber (2021) Effects of COVID-19 on the Musculoskeletal System: Clinician’s Guide 13: 141-150.
- R Pal, M Banerjee (2020) COVID-19 and the endocrine system: exploring the unexplored. J Endocrinol Invest 2: 1-5.
- Mehmet Bostancıklıoğlu (2020) SARS-CoV2 entry and spread in the lymphatic drainage system of the brain. Brain Behav Immun 87: 122-123.
- Benge M dba Miracles (2022) Not Just the Thoracic Duct: A New Understanding of Lymphatic Routing, Chemical & Pharmaceutical Research.
- Yao XH, Li TY, He ZC Y, F Ping, HW Liu (2020) A pathological report of three COVID-19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi 49(5): 411-417.
- Michael Gottlieb, Brit Long (2020) Dermatologic manifestations and complications of COVID-19. Am J Emerg Med 38(9):1715-1721.
- Devon E McMahon, Antonia E Gallman, George J Hruza, Misha Rosenbach, Jules B Lipoff, et al. (2021) Long COVID in the skin: aregistry analysis of COVID-19 dermatological duration. Lancet Infect Dis 21(3): 313-314.
- https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html.
- https://www.cdc.gov/mis/index.html.
- Rodriguez Sanchez I, Rodriguez Mañas L, Laosa O (2022) Long COVID-19: The Need for an Interdisciplinary Approach. Clinics In Geriatric Medicine 38(3): 533-544.
- Vicente Boix, Esperanza Merino (2022) Post-COVID syndrome. The never-ending challenge, Medicina Clínica (English Edition) 158(4): 178-180
- (2022) CDC Centers for Disease Control and Prevention; 2020. COVID-19 and your health.
- Jennifer Graves (2022) CNS Lymphocytic Vasculitis in a Young Woman With COVID-19 Infection. Neurology: Neuroimmunology & Neuroinflammation.
- Riccardo Cau, Gavino Faa, Valentina Nardi, Antonella Balestrieri, Josep Puig, et al. (2022) Long-COVID diagnosis: From diagnostic to advanced AI-driven models, European Journal of Radiology 148: 110164.
- Siny Tsang (2022) Is COVID-19 Keeping us Up at Night? Stress, Anxiety, and Sleep Among Adult Twins. Frontiers in Neuroscience.
- Benjamin ten Oever, Marianna Zazhytska (2022) Non-cell autonomous disruption of nuclear architecture as a potential cause of COVID-19 induced anosmia. Cell.
- Cao X, Li W, Wang T, Dongzhi Ran, Veronica Davalos, et al. (2022) Accelerated biological aging in COVID-19 patients. Nat Commun 13: 2135.
- Aman Y (2022) COVID-19-associated cognitive decline. Nat Aging 2: 275.
- https://neurosciencenews.com/cognition-covid-19054/.
- Hampshire A, Doris A Chatfield, Anne Manktelow MPhil, Amy Jolly, William Trender, et al. (2022) Multivariate profile and acute-phase correlates of cognitive deficits in a COVID-19 hospitalised cohort. eClinical Medicine 47: 101417.
- Adnan I Qureshi, William I Baskett, Wei Huang, S Hasan Naqvi, Chi Ren Shyu (2022) New-Onset Dementia Among Survivors of Pneumonia Associated with Severe Acute Respiratory Syndrome Coronavirus 2 Infection. Open Forum Infectious Diseases 9(4): ofac115.
- https://neurosciencenews.com/mild-covid-brain-shrinkage-20187/.
- Shu Liu André (2021) Highly efficient intercellular spreading of protein misfolding mediated by viral ligand-receptor interactions.
- Adam Hampshire (2021) Cognitive deficits in people who have recovered from COVID-19. E Clinical Medicine.
- S Graves, Jennifer, Garrett Timmons, Annalise E Miner, Visesha Kakarla, et al. (2022) Longitudinal evaluation of neurologic-post acute sequelae SARS-CoV-2 infection symptoms. Annals of Clinical and Translational Neurology 9(7): 995-1010.
- Bernhard A Sabel (2022) Non-invasive brain microcurrent stimulation therapy of long-COVID-19 reduces vascular dysregulation and improves visual and cognitive impairment. Restorative Neurology and Neuroscience.
- Junqueira C, Ângela Crespo, Shahin Ranjbar, Luna B de Lacerda, Mercedes Lewandrowski, et al. (2022) FcγR-mediated SARS-CoV-2 infection of monocytes activates inflammation. Nature 606: 576-584.
- Sefik E, Rihao Qu, Caroline Junqueira, Eleanna Kaffe, Haris Mirza, et al. (2022) Inflammasome activation in infected macrophages drives COVID-19 pathology. Bio Rxiv 606: 585-593.
- Schwabenland M, Salié H (2021) Deep spatial profiling of human COVID-19 brains reveals neuroinflammation with distinct microanatomical microglia-T cell interactions.
- Takumi Satoh (2022) Potential Therapeutic Use of the Rosemary Diterpene Carnosic Acid for Alzheimer’s Disease, Parkinson’s Disease, and Long-COVID through NRF2 Activation to Counteract the NLRP3 Inflammasome.
- https://neurosciencenews.com/pain-long-covid-20306/.
- Odozor CU, Kannampallil T, Abdallah AB, Roles K, Burk C (2021) Post-acute sensory neurological sequelae in patients with SARS-CoV-2 infection: an observational cohort study. Pain.
- https://neurosciencenews.com/covid-19-neuropathy-20255/.
- Tracy Fischer, Ibolya Rutkai, Meredith G Mayer, Linh M Hellmers, Bo Ning, et al. (2022) Neuropathology and virus in brain of SARS-CoV-2 infected non-human primates. Nature Communications 13: 1745.
- Olumayokun A Olajide (2022) SARS-CoV-2 Spike Glycoprotein S1 Induces Neuroinflammation in BV-2 Microglia. Molecular Neurobiology.
- Dervis Salih (2022) Brain A genetic link between risk for Alzheimer’s disease and severe COVID-19 outcomes via the OAS1 gene.
- Steve Reiken, Leah Sittenfeld, Haikel Dridi, Xiaoping Liu, Andrew R Marks (2022) Alzheimer’s-like signaling in brains of COVID-19 patients.
- https://neurosciencenews.com/cognition-covid-19054/.
- Lu Wang, David Sievert, Alex E Clark, Sangmoon Lee, Hannah Federman, et al. (2021) A human three-dimensional neural-perivascular ‘assembloid’ promotes astrocytic development and enables modeling of SARS-CoV-2 neuropathology. Nature Medicine 27: 1600-1606.
- Lu Wang, David Sievert, Alex E Clark, Sangmoon Lee, Hannah Federman, et al. (2021) A human three-dimensional neural-perivascular ‘assembloid’ promotes astrocytic development and enables modeling of SARS-CoV-2 neuropathology, Nature Medicine 27: 1600-1606.
- Myria Petrou (2022) Amyloid deposition in Parkinson Disease and Cognitive Impairment: A Systematic Review. Mov Disord 30(7): 928-935.
- Slav Semerdzhiev, Mohammad AA Fakhree, Ine Segers Nolten, Christian Blum, Mireille MAE Claessens, et al. (2022) Interactions between SARS-CoV-2 N-Protein and α-Synuclein Accelerate Amyloid Formation. ACS Chem Neurosci 13(1): 143-150.
- Mahmoud A Ghannoum, MaryKate Ford, Robert A Bonomo, Ahmed Gamal, Thomas S McCormick, et al. (2021) A Microbiome-Driven Approach to Combating Depression During the COVID-19 Pandemic. Front Nutr 8: 672390.
- Jorge Garza Ulloa (2022) Chapter 7-Cognitive learning and reasoning models applied to biomedical engineering, Applied Biomedical Engineering Using Artificial Intelligence and Cognitive Models. Academic Press pp. 609-676.
- Jorge Garza Ulloa (2022) Chapter 1-Biomedical engineering and the evolution of artificial intelligence, Applied Biomedical Engineering Using Artificial Intelligence and Cognitive Models. Academic Press pp. 1-37.
- Jorge Garza Ulloa (2022) Chapter 3-Artificial Intelligence Models Applied to Biomedical Engineering, Applied Biomedical Engineering Using Artificial Intelligence and Cognitive Models. Academic Press pp. 113-173.
- Jorge Garza Ulloa (2022) Chapter 4-Machine Learning Models Applied to Biomedical Engineering, Applied Biomedical Engineering Using Artificial Intelligence and Cognitive Models. Academic Press pp. 175-334.
- Jorge Garza Ulloa (2022) Chapter 5-Deep Learning Models Principles Applied to Biomedical Engineering, Applied Biomedical Engn eering Using Artificial Intelligence and Cognitive Models. Academic Press pp. 335-508.
- Jorge Garza Ulloa (2022) Applied Biomedical Engineering Using Artificial Intelligence and Cognitive Models, 2021/2022, Academic Press.
- Jorge Garza Ulloa (2022) Chapter 7-Cognitive learning and reasoning models applied to biomedical engineering, Applied Biomedical Engineering Using Artificial Intelligence and Cognitive Models. Academic Press pp. 609-676.
- Frances Stead Sellers (2022) How long covid could change the way we think about disability.
- Kevin da Silva Castanheira, Madeleine Sharp, A Ross Otto (2021) The impact of pandemic-related worry on cognitive functioning and risk-taking. PLOS ONE 16(11): e0260061.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.